Shedding Light on Bacterial Conjunctivitis: Causes, Symptoms, Treatment, and Prevention Strategies
Bacterial conjunctivitis, commonly known as pink eye, is a prevalent ocular condition characterized by inflammation of the conjunctiva. The thin, transparent membrane covering the white part of the eye and inner eyelids. While bacterial conjunctivitis is typically self-limiting and resolves without complications, it can cause discomfort and temporary vision impairment. In this comprehensive guide, we will explore the causes, symptoms, diagnosis, treatment options. And preventive measures for bacterial conjunctivitis, providing valuable insights for both healthcare professionals and individuals affected by this condition.
Understanding:
Bacterial conjunctivitis is primarily caused by bacterial pathogens infecting the conjunctiva, leading to inflammation and ocular symptoms. The most common bacterial agents responsible include:
- Staphylococcus aureus
- Streptococcus pneumoniae
- Haemophilus influenzae
- Moraxella catarrhalis
These bacteria can be transmitted through direct contact with contaminated hands, objects, or respiratory droplets from infected individuals. Factors such as poor hygiene, crowded living conditions, and compromised immune function can increase the risk of bacterial conjunctivitis transmission and incidence.
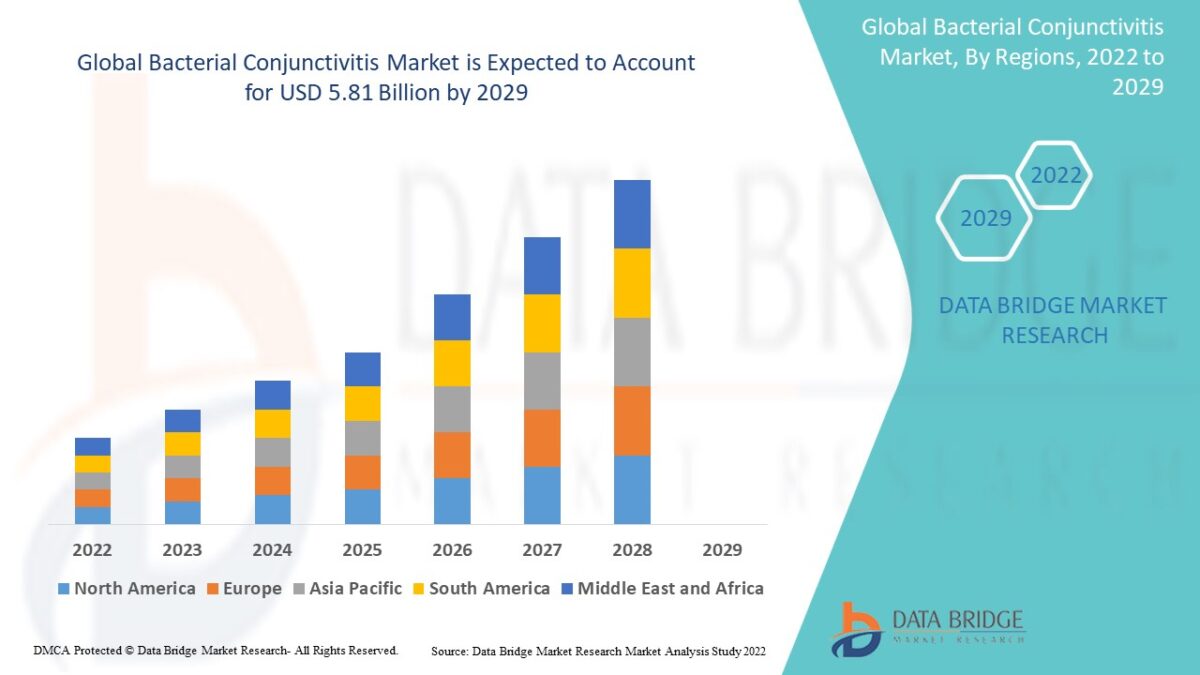
Read More Details: https://www.databridgemarketresearch.com/reports/global-bacterial-conjunctivitis-market
Symptoms:
- Redness (Hyperemia): The conjunctiva becomes inflamed, leading to the characteristic pink or red appearance of the affected eye(s).
- Watery or Purulent Discharge: Bacterial conjunctivitis may produce a sticky, yellowish or greenish discharge, particularly upon waking in the morning.
- Itchiness or Irritation: Individuals with bacterial conjunctivitis may experience itching, burning, or foreign body sensation in the affected eye(s).
- Grittiness or Tearing: Sensations of grittiness, discomfort, or excessive tearing may occur due to inflammation of the conjunctiva.
- Crusting of Eyelids: Dried discharge may accumulate along the eyelid margins, causing eyelids to stick together (especially upon waking).
Diagnosis:
The diagnosis of bacterial conjunctivitis is primarily clinical and based on the presence of characteristic signs and symptoms. However, in some cases, additional diagnostic tests may be performed to confirm the diagnosis or identify the causative pathogen. Diagnostic approaches may include:
- Ocular Examination: A thorough examination of the eyes, including visual acuity assessment, slit-lamp examination, and inspection of the conjunctiva and eyelids, can help identify characteristic signs of bacterial conjunctivitis.
- Microbiological Testing: In cases where the diagnosis is uncertain or when specific bacterial pathogens are suspected, conjunctival swabs or cultures may be obtained for microbiological analysis to identify the causative organism and determine antibiotic susceptibility.
- Differential Diagnosis: Bacterial conjunctivitis should be differentiated from other causes of acute red eye, including viral conjunctivitis, allergic conjunctivitis, and chemical conjunctivitis, based on clinical presentation and history.
Treatment Options:
The management aims to alleviate symptoms, eradicate the causative bacterial infection, and prevent complications. Treatment options may include:
- Topical Antibiotics: Topical antibiotic eye drops or ointments are the mainstay of treatment for bacterial conjunctivitis. Commonly used antibiotics include fluoroquinolones (e.g., ciprofloxacin, moxifloxacin), aminoglycosides (e.g., gentamicin, tobramycin), and polymyxin B/trimethoprim.
- Supportive Therapy: In addition to antibiotic therapy, supportive measures such as warm compresses, artificial tears, and eyelid hygiene may help alleviate symptoms and promote ocular comfort.
- Avoidance of Contact Lenses: Individuals who wear contact lenses should discontinue lens wear during the acute phase of bacterial conjunctivitis to prevent exacerbation of symptoms and reduce the risk of complications.
- Follow-Up: Patients with bacterial conjunctivitis should be monitored closely for treatment response and potential complications. Follow-up visits may be scheduled to assess symptom resolution, evaluate ocular health, and adjust treatment as needed.
Preventive Measures:
Preventing the spread is essential for reducing transmission and minimizing the risk of recurrence. Key preventive measures include:
- Hand Hygiene: Practicing good hand hygiene, including regular handwashing with soap and water, can help reduce the risk of bacterial transmission from contaminated hands to the eyes.
- Avoidance of Eye Rubbing: Avoiding touching or rubbing the eyes with unwashed hands can help prevent the introduction of bacteria into the conjunctival sac.
- Personal Hygiene: Individuals with bacterial conjunctivitis should avoid sharing personal items such as towels, washcloths, and eye makeup to prevent transmission to others and reduce the risk of reinfection.
- Environmental Hygiene: Cleaning and disinfecting frequently touched surfaces and objects, such as doorknobs, countertops, and eyeglasses, can help reduce the spread of bacteria in shared environments.
- Vaccination: Routine vaccination against bacterial pathogens such as Streptococcus pneumoniae and Haemophilus influenzae can help reduce the incidence and other infectious diseases.
Conclusion:
In conclusion, bacterial conjunctivitis is a common ocular condition characterized by inflammation of the conjunctiva due to bacterial infection. While typically self-limiting and benign, It can cause discomfort and inconvenience for affected individuals. By understanding the causes, symptoms, diagnosis, treatment options, and preventive measures, healthcare professionals. And individuals alike can take proactive steps to manage the condition effectively, prevent transmission, and promote ocular health and well-being. Through education, awareness, and adherence to hygienic practices, we can work together to minimize the impact and protect ocular health in our communities.








